
Biofilms as a Cause of Male Infertility
According to the WHO, one out of 5 to 7 couples of reproductive age suffers from infertility today. In half of all cases, the cause is a male factor and a poor quality of sperm in particular. This topic was discussed by leading urologists as part of the Moscow Urological School.
Healthcare professionals have drawn attention to the role of biofilms in fertility disorders in patients with chronic prostatitis.
Biofilms are a relatively new topic for the scientific community; however, it attracts more and more attention of researchers with each passing year. Currently, most fertility disorders in men are associated with inflammation of the prostate gland. Biofilms are formed from so-called «bacterial colonies» and may include proteins, polysaccharides, nucleotides, etc. Biofilms are considered a natural form of microbial existence.
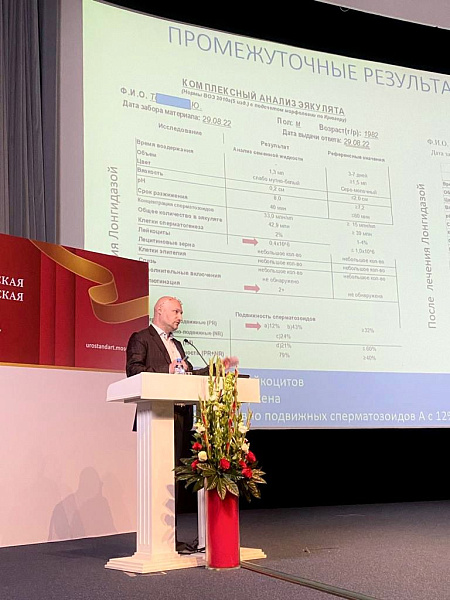
Leonid Spivak, Professor of the Institute of Urology and Human Reproductive Health, Sechenov University, President of the Council of the Association of Conservative Therapists in Urology ASPECT, reported that fertility problems are found in one third of men.
The professor shared a study that found pathogenic bacteria in 33.2 % of the ejaculate samples taken from patients with impaired fertility. In most cases, bacteria in ejaculates are represented by microcolonies; they are covered with a dense microcapsule — one of the biofilm varieties. Bacterial microcolonies can attach to spermatozoa, thereby causing infertility.
1A process by which enzymes help break bonds in molecules.
In the 21st Century Women of Reproductive Age Are More Likely to Suffer from Pelvic Inflammatory Diseases


